Accurate cancer diagnosis and staging are critical for effective patient management. Fdg Pet/CT, or Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography, has become an invaluable imaging technique in oncology for detecting various cancers. This powerful tool combines Positron Emission Tomography (PET) and Computed Tomography (CT) scans, offering synergistic benefits that surpass the limitations of each modality alone. FDG PET/CT plays a significant role in staging and restaging tumors, detecting recurrence, monitoring therapy response, and guiding treatment modifications. It is estimated that in approximately 27% of cases, FDG PET/CT results in a change in patient management. This review aims to provide oncologists, radiotherapists, and clinical specialists with a practical guide to utilizing FDG PET/CT in oncological practice.
Cancer remains a leading cause of mortality globally. Optimal therapeutic strategies depend on precise diagnosis, staging, and restaging of the disease. Positron emission tomography (PET) using 2-deoxy-2-[fluorine-18]fluoro-D-glucose (18F-FDG), a glucose analog, provides crucial functional information. This is based on the principle that cancer cells exhibit increased glucose uptake and glycolysis, allowing FDG PET to identify metabolic abnormalities even before structural changes are visible. Integrated FDG PET/CT systems acquire both PET and CT data simultaneously, enabling precise anatomical localization of lesions detected by FDG PET (). Since its introduction, FDG PET/CT has rapidly become a cornerstone in clinical oncology, establishing itself as a vital imaging modality in routine cancer care ().
Clinical Applications of FDG PET/CT in Oncology
FDG PET/CT’s enhanced sensitivity and specificity in certain cancers have positioned it as a primary tool for staging and restaging, directly influencing patient management. It is also instrumental in differentiating between treatment responders and non-responders early in the therapeutic process, often before tumor size reduction is evident. In specific malignancies such as lymphoma, non-small cell lung cancer, and esophageal cancer, early decreases in FDG PET activity following therapy initiation are strongly correlated with improved survival rates and other clinical outcomes now considered in drug approval processes.
FDG PET/CT is particularly valuable for detecting cancer recurrence, especially in asymptomatic patients with elevated tumor markers and when conventional imaging yields inconclusive results. However, it is important to acknowledge limitations, primarily the non-specificity of FDG uptake and the variable affinity of certain cancers for this tracer. This article will explore the key applications, advantages, and limitations of FDG PET/CT in the field of oncology.
Methodology
This review is based on a comprehensive search of published randomized controlled trials and systematic reviews in English literature. We also included relevant unpublished systematic reviews to ensure a broad perspective. The reviewed publications encompass both retrospective and prospective studies, varying in methodological quality. We evaluated the clinical utility of FDG PET/CT by considering the implications of false-positive and false-negative results and its overall impact on cancer patient management.
FDG PET/CT Applications in Specific Cancers
Breast Cancer
FDG PET/CT is not recommended for primary breast cancer diagnosis due to its limited ability to detect small or non-invasive carcinomas. The sensitivity for tumors smaller than 2 cm is approximately 68%. For axillary nodal staging, FDG PET/CT demonstrates variable sensitivity (79%-94%) and specificity (86%-92%), which is not sufficient for routine clinical application.
Currently, the most significant clinical roles for FDG PET/CT in breast cancer are in detecting and evaluating recurrent or metastatic disease () and in monitoring response to therapy. Patient-based analyses have shown high sensitivity, specificity, and accuracy for FDG PET/CT in detecting locoregional recurrence (89%, 84%, and 87%, respectively) and distant metastases (100%, 97%, and 98%, respectively) (). FDG PET/CT also surpasses the serum tumor marker CA 15-3 in sensitivity for detecting relapsed breast cancer.
In monitoring treatment response, a decrease in the standardized uptake value (SUV) to below 55% of baseline is a strong indicator of histopathological response to chemotherapy in locally advanced breast cancer. Using this criterion, FDG PET/CT has shown high sensitivity (100%), specificity (85%), and accuracy (88%) in identifying responders after the first chemotherapy cycle, with values remaining high after the second cycle (83%, 94%, and 91%, respectively). FDG PET has also demonstrated the ability to predict complete pathological response after a single chemotherapy pulse with 90% sensitivity and 74% specificity. Notably, overall survival rates are significantly lower in FDG PET/CT non-responders (8.8 months) compared to responders (19.2 months). In cases of bone metastases, a positive response can be indicated by reduced FDG activity alongside increased sclerosis on the CT component of FDG PET/CT, suggesting bone healing.
Colorectal Cancer
FDG PET/CT is crucial in colorectal cancer management, particularly for detecting recurrent disease, assessing residual masses post-therapy, localizing recurrence in patients with rising CEA levels, and staging before surgical resection of local or distant recurrence. For detecting intra-abdominal but extrahepatic recurrence, FDG PET/CT exhibits 88% sensitivity, 94% specificity, and 92% accuracy. For extra-abdominal and/or hepatic recurrence, these values are even higher at 95%, 100%, and 99%, respectively. The overall average sensitivity, specificity, and accuracy for detecting recurrent colorectal cancer are reported as 89%, 92%, and 90%, respectively ().
Conventional imaging techniques often struggle to detect local recurrence in the pelvic tumor bed due to residual soft tissue abnormalities post-therapy. However, abnormal FDG activity in residual pelvic soft tissue more than 6 months post-radiotherapy is highly indicative of tumor recurrence, with even greater accuracy and positive predictive value after 12 months. Elevated CEA levels are observed in approximately two-thirds of patients with recurrent colorectal cancer. FDG PET/CT is strongly recommended for patients with unexplained CEA level increases following curative treatment, as it can alter management in a significant proportion of cases (59% to 68%) ().
FDG PET/CT is also emerging as a valuable tool in radiotherapy planning and for predicting and evaluating response to therapy in colorectal cancer. Preoperative radiotherapy planning using FDG PET/CT can significantly modify both gross tumor volume and clinical target volume.
Esophageal Cancer
Endoscopic ultrasound (EUS) remains the standard for local tumor evaluation in esophageal cancer due to its superior accuracy and cost-effectiveness in T-staging and N-staging compared to FDG PET/CT and conventional CT. However, FDG PET/CT plays a critical role in the initial staging of esophageal cancer, specifically in M-staging (). Adding FDG PET/CT to M-staging results in up-staging in 15% to 20% and down-staging in 5% to 7% of patients. Furthermore, synchronous primary tumors, often missed by conventional imaging, are identified in approximately 5.5% of patients through FDG PET/CT.
Assessing tumor response to neoadjuvant therapy with FDG PET/CT is a significant prognostic factor in esophageal cancer, achieving a diagnostic accuracy of around 85%, comparable to EUS and significantly higher than conventional CT. In squamous cell carcinoma of the esophagus and certain inoperable cases, FDG PET/CT is also important for radiotherapy planning, frequently modifying gross tumor volume and planning treatment volume.
For detecting regional and distant recurrences, FDG PET is highly sensitive, with reported sensitivity, specificity, and accuracy of 94%, 82%, and 87%, respectively, outperforming conventional imaging. FDG PET can also detect recurrences in approximately 12% of patients with negative or equivocal findings on conventional imaging.
Head and Neck Cancer
FDG PET/CT significantly impacts the assessment of both newly diagnosed and previously treated head and neck cancer patients. Compared to CT-based evaluation alone, FDG PET/CT alters the initial clinical staging and TNM category in a substantial proportion of patients (14% to 57%) and achieves approximately 90% accuracy in staging, compared to 86% for conventional CT.
For detecting lymph node metastases, FDG PET/CT has a reported sensitivity of 94% and specificity of 84% per patient analysis (), superior to conventional CT. FDG PET/CT also identifies synchronous primary tumors, distant metastases, and the primary site in cases of unknown primary head and neck cancer in a significant percentage of patients. It influences initial management decisions in 18% to 37% of cases and has a crucial impact on radiotherapy planning, changing the plan in approximately 29% of patients and altering gross tumor volume in over half of cases. FDG PET/CT-based assessment often results in a statistically larger gross tumor volume compared to CT-based assessment.
Despite aggressive treatments, locoregional recurrence and distant metastasis remain significant risks in head and neck cancer. FDG PET/CT demonstrates high sensitivity, specificity, and accuracy in restaging these patients. Postoperative, pre-radiotherapy FDG PET/CT evaluation can also alter management decisions in a noteworthy percentage of patients. Furthermore, FDG PET/CT is more accurate than conventional CT when used 4 to 8 weeks post-chemoradiotherapy, with even higher sensitivity and specificity after 8 weeks.
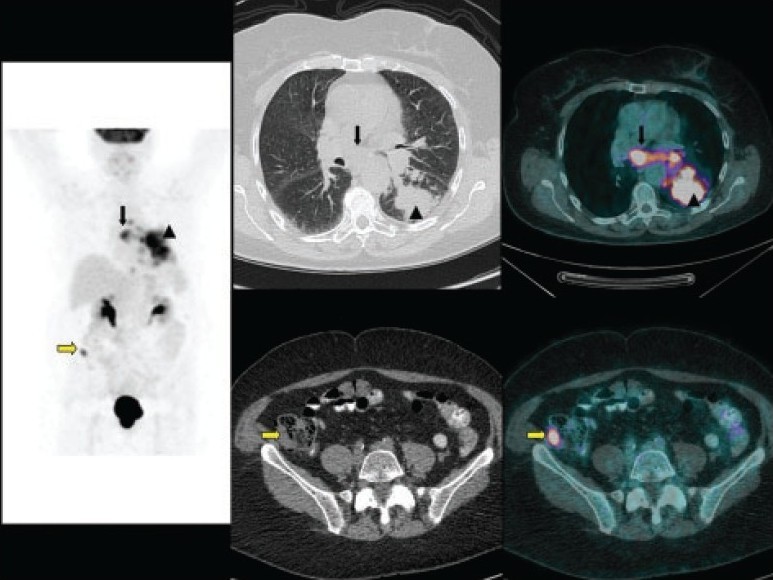
Lung Cancer
Accurate initial staging of non-small cell lung cancer (NSCLC) is essential for determining operability and guiding neoadjuvant treatment. Guidelines recommend FDG PET for non-invasive staging due to the limitations of conventional CT in mediastinal nodal staging. FDG PET/CT is a more accurate method and is becoming the standard for preoperative diagnosis and staging of NSCLC. It changes management in up to 52% of cases and significantly reduces unnecessary thoracotomies.
FDG PET/CT staging in lung cancer has reported diagnostic accuracy and sensitivity for operability of 79% and 64%, respectively, compared to conventional staging. For mediastinal nodal assessment, sensitivity ranges from 67% to 92% and specificity from 82% to 99% () in a significant proportion of asymptomatic patients, preventing futile surgeries.
FDG PET/CT is valuable in radiotherapy planning by providing more accurate staging and allowing the omission of elective radiation to uninvolved nodal stations. Its CT component can also be utilized for radiotherapy planning. In limited-stage small cell lung cancer, FDG PET/CT can modify treatment fields significantly. For post-treatment evaluation, FDG PET/CT is more accurate than conventional CT in detecting residual and recurrent disease, guiding treatment decisions. It demonstrates high sensitivity and specificity for detecting recurrent NSCLC. Residual FDG uptake post-treatment is associated with poorer prognosis.
Reduction in baseline maximum SUV on FDG PET is predictive of complete pathologic response with high sensitivity, specificity, and accuracy. For indeterminate solitary pulmonary nodules (SPNs), FDG PET/CT is reserved for cases where CT-guided biopsy is technically challenging or non-diagnostic. FDG PET has similar sensitivity but better specificity than CT in characterizing malignancy in SPNs.
Lymphoma
FDG PET/CT is now a standard tool for initial staging, therapy response monitoring, and restaging in Hodgkin lymphoma (HL) and high-grade non-Hodgkin lymphoma (NHL). Its clinical utility varies by pathological subtype, but not necessarily tumor grade. FDG PET/CT shows superior sensitivity and specificity in disease assessment for HL compared to conventional CT alone. In HL or high-grade NHL, FDG PET/CT exhibits high sensitivity and specificity for both lymph node and organ involvement ().
False-negative FDG PET scans can occur in MALT lymphomas due to their lower metabolic activity. Aggressive NHL typically shows more intense FDG activity than lower-grade NHL, although overlap exists. FDG-avid lesions in low-grade NHL should raise suspicion of transformation to higher-grade lymphoma. False-positive FDG PET/CT scans can be caused by infectious or inflammatory diseases, which should be considered during interpretation.
Residual post-therapy masses are common in lymphoma. Interim FDG PET/CT results (after a few chemotherapy cycles) are strongly correlated with event-free survival in HL () and high-grade NHL. Negative interim PET results are associated with significantly higher event-free survival rates compared to positive interim PET results.
Thyroid Cancer
Differentiated thyroid cancers, mainly papillary and follicular carcinoma, constitute the majority of thyroid malignancies. De-differentiated thyroid cancer cells may lose radioiodine concentrating ability. FDG PET demonstrates high sensitivity in patients with elevated thyroglobulin and negative 131I whole-body scans. In this specific group, FDG PET/CT can alter clinical management in a significant percentage of patients.
Urological Cancer
Renal Cell Carcinoma
FDG PET/CT has limited sensitivity for evaluating metastatic renal cell carcinoma (RCC), especially for small lesions. However, a positive FDG PET/CT scan is highly suspicious for recurrence or metastasis due to its high specificity and positive predictive value. Combining PET with contrast-enhanced CT may be necessary for critical management decisions.
Prostate and Bladder Cancer
FDG PET/CT is not currently established for prostate or bladder cancer assessment due to low accuracy. This is attributed to the low metabolic rate of prostate cancer and tracer excretion interference in bladder cancer. However, newer PET radiotracers like 11C-choline and 18F-fluorocholine show promise in prostate cancer management.
Gynecological Cancers
Cervical Cancer
FDG PET(/CT) plays a major role in preoperative staging of advanced cervical cancer and restaging post-treatment. It demonstrates high sensitivity, specificity, and accuracy for detecting para-aortic nodal metastases in advanced cervical cancer. Preoperative FDG PET influences patient management in a notable percentage of cases. In recurrent cervical cancer, FDG PET also shows high sensitivity and specificity. Post-treatment FDG PET results are prognostic for progression-free survival.
Ovarian Cancer
FDG PET(/CT) is crucial in evaluating recurrent ovarian cancer, particularly when serum CA-125 levels are elevated and conventional imaging is inconclusive. It exhibits good sensitivity and positive predictive value for detecting recurrent disease of a certain size.
Cutaneous Melanoma
FDG PET/CT is not recommended for early-stage cutaneous melanoma. However, in advanced and recurrent melanoma, FDG PET demonstrates high sensitivity for visceral and abdominal nodal metastases and high accuracy for superficial lymph node metastases. FDG PET can lead to changes in staging and overall management in a significant proportion of patients.
Brain Tumors
FDG PET/CT has relatively lower sensitivity and specificity in evaluating low-grade and recurrent brain tumors and treatment-induced changes due to high physiological brain FDG uptake. Co-registration with MRI and delayed imaging can improve accuracy. FDG PET/CT can identify anaplastic transformation in low-grade tumors and has prognostic value.
Pitfalls of FDG PET/CT
Interpreting FDG PET/CT scans requires awareness of potential pitfalls. Tumor detection is influenced by factors like size, metabolic activity, background activity, and serum glucose levels. False-negative results can occur in small lesions, tumors with low metabolic rates, with interfering cytostatic treatments, and in poorly prepared patients with glucose intolerance (). High physiological FDG activity can also mask lesions.
False-positive results can arise from increased FDG uptake in activated macrophages, neutrophils, fibroblasts, and granulation tissue associated with infectious/inflammatory processes, post-surgical changes, and post-radiation changes.
Future Directions of FDG PET/CT
The evolving role of FDG PET/CT includes evaluating early therapy response, an area where effective imaging tools are still needed. FDG PET/CT shows promise in predicting therapy response and hard endpoints like time to progression. Further large clinical studies are likely to expand its clinical applications in this context. While FDG is the predominant tracer, development and clinical adoption of tracers targeting tumor angiogenesis, hypoxia, proliferation, and receptors are expected to increase.
Conclusion
FDG PET/CT is an established and powerful imaging modality in oncology. Its applications span across various cancer types and clinical scenarios, including staging, restaging, recurrence detection, and therapy response assessment. While recognizing its limitations and potential pitfalls is crucial, FDG PET/CT significantly contributes to improved cancer management and patient outcomes. Continued research and development of novel tracers and applications will further solidify its role in the future of oncology.